In 1968, thirteen men gathered at the Harvard Medical School to virtually undo 5,000 years of the study of death. In a three-month period, the Harvard committee (full name: the Ad Hoc Committee of the Harvard Medical School to Examine the Definition of Brain Death) hammered out a simple set of criteria that today allows doctors to declare a person dead in less time than it takes to get a decent eye exam. A good deal of medical language was used, but in the end the committee’s criteria switched the debate from biology to philosophy. Before many years went by, it became accepted by most of the medical establishment that death wasn’t defined by a heart that could not be restarted, or lungs that could not breathe. No, you were considered dead when you suffered a loss of personhood.
But before we see what substituting philosophy for science actually means to real patients, let’s look at the criteria the Harvard authors believed indicated that a patient had a “permanently nonfunctioning brain”:
- Unreceptivity and unresponsivity. “Even the most intensely painful stimuli evoke no vocal or other response, not even a groan, withdrawal of a limb or quickening of respiration,” by the committee’s standard.
- No movements or spontaneous breathing (being aided by a respirator does not count). Doctors must watch patients for at least one hour to make sure they make no spontaneous muscular movements or spontaneous respiration. To test the latter, physicians are to turn off the respirator for three minutes to see if the patient attempts to breathe on his own (the apnea test).
- No reflexes. To look for reflexes, doctors are to shine a light in the eyes to make sure the pupils are dilated. Muscles are tested. Ice water is poured in the ears.
- Flat EEG. Doctors should use electroencephalography, a test “of great confirmatory value,” to make sure that the patient has flat brain waves.
The committee said all of the above tests had to be repeated at least 24 hours later with no change, but it added two caveats: hypothermia and drug intoxication can mimic brain death. And since 1968, the list of mimicking conditions has grown longer. Although the Harvard criteria were based on zero patients and no experiments were conducted either with humans or animals, they soon became the standard for declaring people dead in several states, and in 1981, the Uniform Determination of Death Act (UDDA) was sanctioned by the National Conference of Commissioners on Uniform State Laws. The UDDA is based on the Harvard Ad Hoc Committee’s report. That a four-page article defining death should be codified by all 50 states within 13 years is staggering. Just as some of our ancestors saw the heart as the locus of the soul, today the medical establishment assumes that the brain is what defines humanity and that a functioning brain is vital to what is called a human being’s personhood. D. Alan Shewmon, a pediatric neurologist at UCLA who was originally pro–brain-death, now dismisses the idea. The most scientific approach one can take to death, he says, is to treat human beings like any other species. People should be judged biologically on whether they are alive or dead, not on some vague notion of personhood. There is no abstract notion of “squirrelness,” for example, or “gorillahood,” by which we determine the death of other species. The question is: Why do we even need concepts like personhood and brain death? Despite heroic efforts to clarify and justify the Harvard criteria, they remain opaque, confusing, and contradictory. If, as proponents say, brain death criteria describe the same condition—i.e., death—as the cardiopulmonary criteria, why bother? Especially since the tools are available for declaring cardiopulmonary death, and are sorely lacking, or at least ignored, for determining whether the whole brain is really dead.
Shewmon compiled 150 documented cases of brain-dead patients whose hearts continued to beat, and whose bodies did not disintegrate, past one week’s time. In one remarkable case, the patient survived 20 years after brain death before succumbing to cardiac arrest.
Brain-death advocates have always insisted that anyone who meets their criteria will fall apart quickly, and go quickly to meet the cardiopulmonary criteria. Yet Shewmon presents a litany of life processes that brain-dead patients continue to exhibit:
- Cellular wastes continue to be eliminated, detoxified, and recycled.
- Body temperature is maintained, though at a lower-than-normal temperature and with the help of blankets.
- Wounds heal.
- Infections are fought by the body.
- Infections produce fever.
- Organs and tissues continue to function.
- Brain-dead pregnant women can gestate a fetus.
- Brain-dead children mature sexually and grow proportionately.
So what drove the Harvard Ad Hoc Committee to turn back the calendar and construct a lower standard for death? To a growing number of scientific critics it appears that the committee was fixated on freeing up human organs for transplant. By the 1960s, thanks to significant advances in technology, these kinds of transplants—once a staple of science fiction—had become a practical reality. But to accomplish this morally and legally, a new definition of death, one that enabled the organs to remain viable, had to be created. Today the transplant industry is a $20 billion per year business. It spends more than a billion dollars a year on immunosuppressive drugsalone, which prevent the recipient’s immune system from rejecting the transplanted organ. Transplant surgeons are near the top of the M.D. food chain, earning on average around $400,000 per year. They and their staffs often fly to organ harvests on private jets. Finder’s fees, in the form of “administrative costs,” are often paid to hospitals. The only people who do not get a share of the transplant wealth are the most essential: the donors and their families. By law, they are the only ones who cannot be compensated. Joseph Murray, the surgeon who performed the first solid-organ transplant, maintains that donors must not be paid, in order to maintain the integrity of the field. It is the job of organ procurement organizations and their wranglers to talk a family out of the organs belonging to a soon-to-be-dead son, daughter, husband, wife, nephew, niece, or other relative. This must be one of the toughest sales jobs in the world. Distraught parents whose child is dead or dying must be asked to make yet another sacrifice. But it is that very pain and confusion that helps organ procurement organizations ease their way in. Jim McCabe, senior donation coordinator for the New England Organ Bank, explains that “it’s a way of finding meaning in death, make the best of a tragic situation. I’m going into the ICU to offer the family an option.” The option most families want is to keep their loved one alive. A brain-death team tells them that survival is not in the cards. Then McCabe gives them another option: to keep someone else alive. His batting average is excellent. He gets 50 to 60 percent of next of kin to agree. Joanne Lynn, M.D., a geriatrician and director of the Altarum Center for Elder Care and Advanced Illness based in Washington, D.C., says, “Advocate groups just want the organs. Transplant debate has ignored the donors and focused on the recipients.” Organ transplants would be peripheral to the story of death if they were what the organ trade claimed them to be: the neat extraction of body parts from totally dead, unfeeling corpses. But it is more complicated and messier than that. The grisly facts compiled in this article are not an attempt to derail organ transplantation—an impossible task, given how entrenched the industry is—but knowledge that has been gained from the medical establishment’s obsession with recycling the bodies of people who are, in the words of Dr. Michael DeVita of the University of Pittsburgh’s Medical Center, only “pretty dead.” Or if you want to take a more optimistic point of view, these facts are proof of the tenacious persistence of human life. Despite the Harvard Ad Hoc Committee’s claims that its criteria for brain death and the cardiopulmonary criteria describe the same phenomenon, beating-heart cadavers (BHCs) are decidedly different from regular corpses. “I like my dead people cold, stiff, gray, and not breathing,” says DeVita. “The brain dead are warm, pink, and breathing. They look sick, not dead.” Beating-heart cadavers were created as a kind of subspecies designed specifically to keep organs fresh for their future owners. McCabe says keeping the body alive from the brain stem down defeats warm ischemia, the restriction or loss of blood flow after conventional death. When the circulation stops, oxygen is no longer delivered to the organs, and cells begin to die.
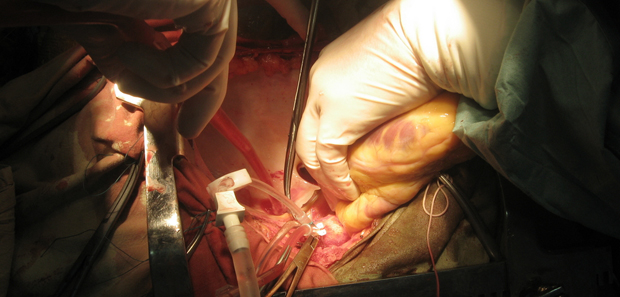
McCabe says his outfit can get a donor from brain death to the operating room in 12 hours. Sometimes it may take an hour after death is declared to obtain consent, the ventilator being kept on while negotiations continue. An hour later, a blood sample is drawn, and it takes eight hours to check for AIDS, hepatitis, and cancer, all of which disqualify a BHC from becoming a donor. Time is of the essence, because the beating-heart cadaver—a brand new kind of creature, known only since the advent of brain death—could easily have a heart attack and die again before his organs are removed. Once a patient goes brain dead, and relatives sign his organ donation consent form, he will get the best medical care of his life. Code blues in hospitals may be a call for doctors to rush to the bedside of beating-heart cadavers who need their hearts defibrillated. BHCs are also routinely turned in their beds so they don’t get bedsores. Their kidneys are treated to avoid renal failure. Fluids are administered constantly to avoid diabetes insipidus, among other things; a healthy BHC should pee out 100 to 250 milliliters of urine per hour. The lungs have to be monitored to keep them in shape for the next owner, and mucous is removed. Steven Ross of Cooper University Hospital in Camden, New Jersey, and Dan Teres of Baystate Medical Center in Springfield, Massachusetts, both say keeping BHCs “alive” is an arduous task for hospital nurses and other workers. Ross says it takes “very aggressive care.” But that they can be medically cared for at all, as Alan Shewmon demonstrated with his 150 cases, gives one pause about the validity of their deaths. There is more than one way to harvest a beating-heart cadaver. McCabe’s outfit uses a team of seven in the operating room: one surgeon, one resident, one technician from the organ bank, one coordinator from the ICU, two nurses, and one anesthesiologist. Some teams may add another surgeon if many organs are being extracted. In a typical dissection, a midline incision is made from just below the neck to the pubic area. The sternum is split with an electric saw or a Lebsche knife, a chisel-like instrument the doctor hits with a mallet. A sternal retractor with spikes is used to open the sternum. Sometimes the aorta is clamped at the beginning of the harvest, and the blood replaced with a coolant to avoid clots and stabilize temperature. Traditionally, the donor’s blood is simply left in place. Mark Schlesinger does not like his patients to feel pain during conventional surgery. He is chairman of the department of anesthesiology at Hackensack University Medical Center in New Jersey, and he points out that an anesthesiologist creates brain-dead patients every day: “We give drugs to make them die. And we bring them back [when the surgery is completed].” A patient under anesthesia is one of the many growing exceptions to the Harvard criteria. He would meet the criteria on the surface, but would be disqualified (ruled still alive) if the examining doctor knew his system was full of drugs. “The only test you fail under anesthesia,” Schlesinger says, “is irreversibility.” That is, if an anesthetized patient has had his brain stem put down temporarily. A brain-dead organ donor’s brain stem is also down—but we do not know, given the limitations of the Harvard criteria and their focus entirely on the brain stem, what is going on with the donor’s cerebral cortex or everything beyond the brain stem. Anesthesiologists have been at the forefront of questioning the finality of brain death and whether beating-heart cadavers truly are unfeeling, unaware corpses. They have also begun wondering about what a “pretty dead” donor may experience during a three- to five-hour harvest sans anesthetic, and they are speaking out on the subject. Gail A. Van Norman, a professor of anesthesiology and bioethics at the University of Washington, cites some disturbing cases.
In one, an anesthesiologist administered a drug to a BHC to treat an episode of tachycardia during a harvest. The donor began to breathe spontaneously just as the surgeon removed his liver. The anesthesiologist reviewed the donor’s chart and found that he had gasped at the end of an apnea test, but a neurosurgeon had declared him dead anyway. In another case, a 30-year-old patient with severe head trauma was declared brain dead by two doctors. Preparations were made to excise his organs. The on-call anesthesiologist noted that the beating-heart cadaver was breathing spontaneously, but the declaring physicians said that because he was not going to recover he could be declared dead. The harvest proceeded over the objections of the anesthesiologist, who saw the donor move and react to the scalpel with hypertension that had to be treated. It was in vain since the proposed liver recipient died before he could get the organ, which went untransplanted. And in a third instance, a young woman suffered seizures several hours after delivering her baby. A neurologist said it was a “catastrophic neurologic event,” and she was readied for harvest. At that time the anesthesiologist found that she had small yet reactive pupils, weak corneal reflexes, and a weak gag reflex. After treatment, “the patient coughed, grimaced, and moved all extremities.” She regained consciousness. She suffered significant neurologic deficits but was alert and oriented.
The brain-death establishment discounts such stories as “anecdotal,” as if they were taken from the National Enquirer. But these three cases appeared in Anesthesiology, the journal of the American Society of Anesthesiologists, which has 44,000 members. The Harvard criteria state that the brain-dead patient must exhibit no movement. Van Norman, however, points out that some exhibit spinal automatism, a complex spectrum of movements including flexion of limbs and trunk, stepping motions, grasping motions, and head turning. Dr. Gregory Liptak, in the Journal of the American Medical Association, wrote: “Patients who are brain dead often have unusual spontaneous movements when they are disconnected from their ventilators…. Goose bumps, shivering, extensor movements of the arms, rapid flexion of the elbows, elevation of the arms above the bed, crossing of the hands, reaching of the hands toward the neck, forced exhalation, and thoracic respiratory-like movements… These complex sequential movements are felt to be release phenomena from the spinal cord including the upper cervical cord and do not [emphasis author’s] mean that the patient is no longer brain dead.” One cannot determine with certainty what organ donors feel, if anything, while being harvested. The logic of brain death goes like this: If the brain stem is dead, then the higher centers of the brain are also probably dead, and if the whole brain is
dead, then everything beneath the brain stem is no longer relevant. Since in practice only the brain stem is routinely tested, the vast majority of the body, everything above the brain stem and everything below, no longer counts as human. The reason for denying beating-heart cadavers anesthetic during the removal of their organs is hard to pin down. (Some experts say it is because anesthetic will harm the organs.) Nevertheless, administering anesthetics to BHCs during organ harvests is becoming more common in Europe, according to Robert Truog, professor of medical ethics, anesthesia, and pediatrics at Harvard Medical School. Despite their strong opposition to brain death, Truog and Shewmon both refuse to acknowledge the possibility that some donors may be in severe pain during organ harvests, even though they acknowledge that some donors did exhibit reactions similar to inadequately anesthetized surgical patients who afterward reported pain and consciousness. Shewmon said the donor reactions were simply “bodily reactions to noxious stimuli.” I asked if an experiment could be designed to answer the question of pain in donors. He said no. Truog did not even want to discuss the possibility of pain in the organ donor. But when I suggested experiments along the lines suggested by other anesthesiologists—when BHCs show pain reactions during a harvest, administer anesthetic to see if the reactions subside—he surprised me by saying he had already done this. He has used two different kinds of anesthetics that do not harm organs to quell symptoms such as high blood pressure or heart rate. “Just because the symptoms come down, though,” he added, “does not mean the patient is in pain. Pain is a subjective thing.” As with Shewmon, I asked Truog if an experiment wasn’t called for. He said there was no experiment that could answer the question of pain in the donor.
Beyond pain, there are many surprising findings in a 1971 paper, “Brain Death: A Clinical and Pathological Study,” published in the Journal of Neurosurgery. The Minnesota team that produced that article studied 25 moribund patients, conducting autopsies on them all and EEGs on some. They also checked for reflexes and found something unusual. Five of the 25 brain-dead people were still sexually responsive. The researchers gently stroked the “nipple and areola” of all patients and got responses from five, four men and one woman. Then they stroked the skin at the root of the penis on the 18 male patients, and four responded with “gentle seesaw movements of the penis.” The researchers felt this reaction was “an incomplete or abortive form of penile erection.” Abortive or not, to the untrained eye it would appear to be a sign of life.
More dramatic are brain-dead pregnant women. The first recorded case occurred in 1981 when a 24-year-old woman, 23 weeks pregnant, was admitted to the Women and Children’s Hospital of Buffalo. After 18 days her EEG showed no cerebral activity and she was transferred to a maternity hospital. A day later she was declared brain dead, approximately 25 weeks pregnant. So she was dead but still pregnant, and doctors decided to use her body—technically it was a corpse—as an incubator. The task was not easy. She developed diabetes insipidus, sinus tachycardia, and uterine contractions. Later she had wide fluctuations in blood pressure, and the fetus’s heart rate was dropping. A cesarean section was performed immediately, delivering a 2-pound “vigorous” baby girl at about the 26th week of gestation. Three months later the infant was discharged from the hospital, weighing about 4.4 pounds.
Six months earlier, another pregnant woman in desperate straits was admitted to the same hospital, with a very different ending. The doctors discontinued life support short of brain death as the fetus was 19 weeks old, and the medical staff accepted the belief that a body could not survive long after brain death was declared. There was theoretically not time to gestate the fetus another 3 weeks, 22 weeks being the earliest a viable baby can be delivered. More brain-dead pregnant moms followed. As of this writing there have been 22 published reports from around the world, including Brazil, Germany, Ireland, New Zealand, France, Finland, Korea, Spain, and the United States. From these 22 brain-dead mothers, 20 babies were produced, with no remarkable side effects in the infants. One woman gestated a fetus for 107 days after declaration of brain death. The real significance of pregnant brain-dead women is that they would seem to sound the death knell for brain death as a definition. As Shewmon and many others have pointed out, what is more indicative of life than gestating a baby to a live and viable birth? Keeping a pregnant mother and baby “alive” for 107 days at the very least puts the lie to the theory that the brain dead will go quickly to conventional heart/lung death. At first, brain death advocates said this is a matter of hours. Then they said 3 to 5 days at the most. Then 7 days, then 9 days, then 14 days. Now we are talking about a brain-dead mother not only hanging on for 107 days but nourishing a baby as well.
A final note: Brain-dead mothers can still donate their organs. And so, after suffering a neurological catastrophe, being declared dead, still having to endure several weeks of pregnancy, then giving birth via cesarean section, the patient can still be rolled off to have her organs removed. A woman’s work is never done.